Germany Surgery – 1 Year Update & What’s Next
Exactly one year ago today, on August 3, 2022, I was in an operating room in Germany (4,143 miles from home) for 7 hours to fix 3 out of 4 of my vascular compressions!

I didn’t have proper blood flow to my celiac artery, renal vein, superior mesenteric artery and left iliac vein which caused pain, extremely low blood pressure, headaches and a gazillion other symptoms. These are all abdominal vascular compressions that carry blood and oxygen to your stomach, kidney, duodenum, colon and other important areas of your GI system.
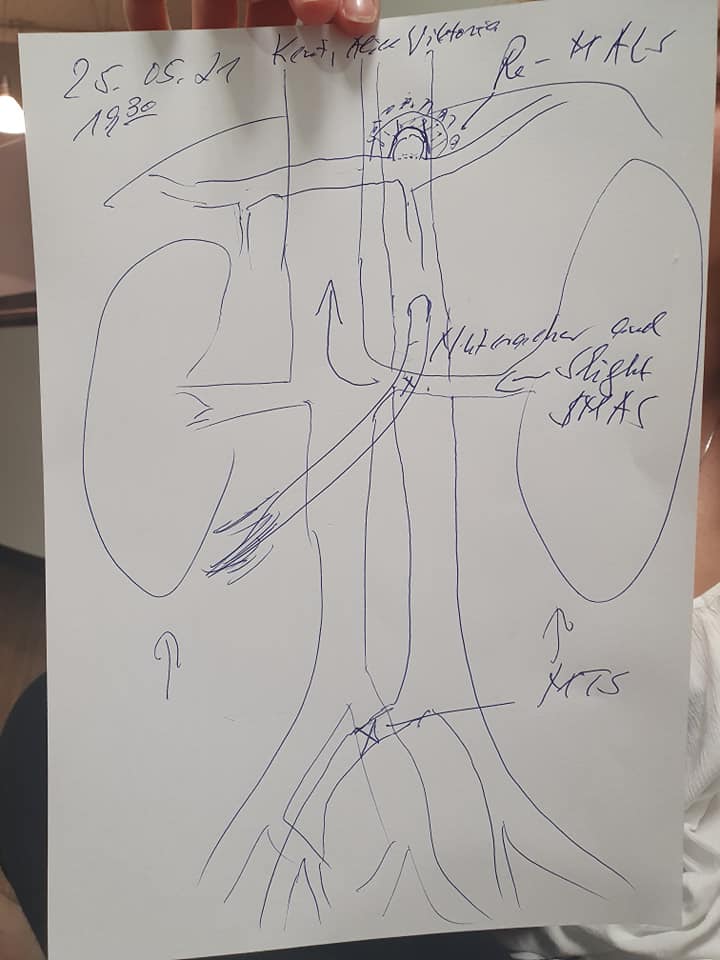
My surgical team was attempting to fix Median Arcuate Ligament Syndrome (MALS), Nutcracker Syndrome (NCS) and Superior Mesenteric Artery Syndrome (SMAS). I was also supposed to have my severe May Thurner Syndrome (MTS)/iliac birth anomaly fixed, but it couldn’t be done due to time constraints.

During surgery I had…
- An external stent placed around my compressed anterior renal vein and my compressed posterior renal vein was ligated.
- The external stent also “propped up” my SMA.
- A partial MALS resection.
- A left kidney Nephropexy. My kidney “pinned” under my ribs because of nephroptosis aka “floating kidney”.
The estimated full recovery time for this surgery is one year and I’ve finally met this time frame. I hoped and prayed that I’d be writing a much different update than I’m writing today.
So did the surgery work and am I better?
Yes, the surgery fixed my renal vein and celiac artery blood flow.
No, I am not better. In fact, I’m actually much worse.
There are believed to be 4 main reasons why I’m doing worse…
1. Renal Vein Stent: The doctors we’ve consulted with believe the stent around my renal vein for NCS is too big for my body and in a spot where I just don’t have room for it. Because of hypermobility EDS (a connective tissue disorder), it’s partially collapsing into my aorta and pushing against my superior mesenteric artery and inferior vena cava in ways it shouldn’t be.
Whenever my heart beats, it pushes the stent against my arteries causing inflammation, nerve pain and is most likely the cause of my scary low blood pressure (it got down to 60/40 recently in the hospital!!!) and worsening POTS and Dysautonomia symptoms.
The worst part is that I’m in a TON of pain. So much more pain than I had before surgery. The worst of the stent pain happens when I try to sit up completely or stand, so I can only walk or sit upright for a few minutes before my lower back, abdomen and the area below my ribs start to burn and cause incredible stabbing pain. Unfortunately this means anytime we go out of the house or for walks I need to use a wheelchair.

I was able to stand, walk and sit for much longer periods of time prior to my surgery. The only way I get a little relief from the stent pain right now is by lying flat or sitting in a reclined position with my legs up.
2. Iliac Vein Compression. My iliac vein compression was NOT fixed during surgery due to time constraints and I have zero blood flow going through my left iliac vein. This is causing severe pelvic, lower back and leg pain. Because my iliac veins scarred together at birth instead of separating like they’re supposed to, my body created LOADS of collaterals. Some are going up my spine which is causing my daily head and neck pain.
3. MALS Release: There are different schools of thought with MALS pain. That the actual compression is causing the pain, that surround irritated nerves are causing neurogenic pain or that BOTH the compression and the surrounding irritated nerves are causing pain. During my surgery only the nerves in the way of the compression were addressed. It appears on my CT prior to surgery that I had a lot of irritated nerves wrapping around my celiac artery and aorta and so some of those nerves remain. Some surgeons believe I still have a neurogenic pain component, meaning the remaining irritated compressed nerves are causing my continued pain.
4. Aggravated GI Symptoms. Ever since surgery I’ve been experiencing severe abdominal swelling which has made my nausea and abdominal pain much worse. Prior to surgery I was able to at least tolerate enough J-feeds to sustain my weight and hydration status.
Since surgery, my belly swells huge with any oral intake or J-feeds. This adds to my pre-existing pain and nausea which also isn’t any better. During a recent 6 week hospital admission, we figured out that if I drain from my G-port 24/7 it somewhat reduces my stomach swelling so I can tolerate J feeds better. So far, the abdominal swelling remains a mystery to my surgeon plus all the GI and motility doctors we’ve consulted with. Some think the stent could be contributing to this because it wasn’t an issue pre-op and it appears to be significantly pushing up on my superior mesenteric artery, but they are not entirely sure so no one really knows how to help me with this particular issue. My motility specialist keeps telling me “you’re a complicated young lady”. Does anyone like to hear that? No!
Having conditions like hyper-mobility EDS, Gastroparesis, POTS, Dysautonomia (Autonomic Dysfunction) and Colonic Neuropathy all make my situation and recovery more complex.
SO…. What’s Next?
Remove Stent and Auto-Transplant Kidney
We have been advised by multiple doctors that I need to get the stent OUT as soon as possible. There are only two surgeons in the entire US who have removed this type of stent. The surgeon we think we’re going to proceed with said there will be a lot of scar tissue, adhesions and inflammation all of which will make the stent removal difficult and risky and there is no guarantee he will even be able to get it out.
To add to the complexity of the situation, removing the stent will give me full blown Nutcracker Syndrome (NCS) and Superior Mesenteric Artery Syndrome (SMAS) again. To fix NCS, the surgeon will need to auto-transplant my kidney to a new place inside my body where the blood flow won’t be impaired. Because of my connective tissue disorder, this could potentially cause a slew of new complications. We don’t know the solution for SMAS yet and need to have more discussions because it’s a complicated situation.
This would be another major open abdominal surgery and we’d need to be away from home for another 6 weeks. Sigh… We are planning on meeting the surgeon in person later this month to go over every little detail and work out the logistics because at this point we’ve only had zoom calls with him. If the surgery at least takes away the stent and NCS pain, I will consider it to be a win. I can’t wait for the day I can stand and sit without pain!!! It can’t come soon enough!!!
Fix May Thurner/Iliac Vein Compression
After the stent removal and autotransplant, I will need my May Thurner compression addressed. There’s no blood flow going through my left iliac vein which has caused my body to create a load of collaterals and creates a high risk for a DVT. One collateral is traveling up my spine causing daily headaches and neck pain. Several doctors have told us I have “the most impressive” case of May Thurner they’ve ever seen. My iliac vein (according to my venogram) is 100% blocked. The fix is either a stent, which isn’t a great option because it could potentially migrate and I’ll probably outgrow it, but would be a minimally invasive procedure OR an iliac vein bypass, which would be another major surgery with a long recovery period.
Fixing the iliac vein compression could potentially help with a lot of my GI issues. There isn’t much documented yet, but one of the vascular surgeons we’ve consulted with has seen many patients whose GI symptoms have resolved once their iliac vein compression was relieved. This would be amazing!!!
MALS Revision
After all of this, if my MALS pain and symptoms persist, I will need revision surgery to address the irritated nerves surrounding my celiac artery.
I Won’t Give Up!
Amazingly, we met an awesome doctor who helped us map out the steps above that are needed for my journey to recovery. He believes he can help me get my health back!! This seems like such a simple thing for a doctor to do, but trust me it’s NOT! Most doctors only specialize in one area and aren’t willing to look at the big picture and how all the pieces of the puzzle fit together and can affect each other. It almost feels like a miracle when you find one who is willing to be your “quarterback”.
This has been such a long and complicated 5 year journey that started in 2017. We went into my surgery last summer thinking that by this summer I’d be living a mostly normal, pain and symptom free life without my feeding tube or the addition of a port. There are days when it’s been hard to accept that this didn’t happen.
For now, while I’ll still be sitting on the sidelines, I won’t give up! I’m incredibly grateful for all the people I’ve connected with along the way… especially the caring nurses and supportive patients from all over the world who have become my friends. Thank you for supporting me and keeping me in your prayers!
Much love to you all!
Grace


Hi Grace…
Thank you for sharing your journey. I am so sorry you’ve had to deal with these issues for so long! 🙁
I am just starting a similar journey although nowhere near what you’ve been through. Would you be willing to share the name of the amazing doctor you’ve found?
Thank you! I have a daughter also named Grace, so we are both sending you love and light. 🙂
Oh Grace…there are no words to express how sorry I am that you have had to endure this for the last 5 years. I want to thank you for telling the whole story and bringing awareness to vascular compressions and the complications they bring. So complicated that very few doctors know how to deal with it. That is crazy. You are an inspiration to others, and your mom is amazing for the fight she has put up on your behalf. Love you so much!
Grace you and your family continue to be in my prayers and I will be keeping my fingers and toes crossed for this next procedure and beyond! Thank you for the update!!! Is there anything I can do to support you?